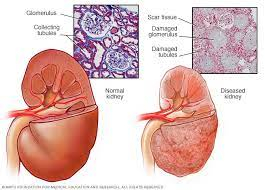
• Chronic renal failure (CRF) is defined as irreversible deterioration in renal function over 3 months with GFR <15/minute/1.73 m2
Causes
• Primary or secondary glomerulonephritis
• Diabetic nephropathy
• Hypertensive nephrosclerosis
• Polycystic kidney disease
• Chronic pyelonephritis
• Tubulo-interstitial diseases
• Analgesic nephropathy
• Vesicoureteric reflux
• Renal tuberculosis
• Nephrocalcinosis
• Obstructive uropathy
Clinical Features
• Anorexia, nausea and vomiting are usually attributed to the formation of ammonia from urea in the upper gastrointestinal tract.
• Anaemia in CRF is normochromic and normocytic in type, and is primarily due to reduced erythropoietin production by the kidney.
• The term renal osteodystrophy embraces various forms of bone disease that develop in CRF. Renal osteodystrophy includes osteomalacia, hyperparathyroid bone disease (osteitis fibrosa), osteoporosis and osteosclerosis.
• Generalised myopathy is due to a combination of poor nutrition, hyperparathyroidism and vitamin D deficiency.
• Neuropathy may be motor, sensory or autonomic.
• Endocrine abnormalities include amenorrhoea in females and loss of libido in both sexes.
• Pericarditis is a common cardiovascular complication in untreated end-stage renal failure.
• Hypertension develops in approximately 80% of patients with CRF.
• Metabolic acidosis is a common accompaniment of CRF.
• Electrolyte abnormalities particularly hyperkalaemia, hypocalcaemia and hyperphosphataemia.
• Patients with CRF have increased susceptibility to infections due to impaired cellular and humoral immunity.
• In addition, uraemia can affect the lung ("uraemic lung") and brain ("uraemic encephalopathy").
• Frequently patients complain of pruritus, often intractable.
• Dialysis dementia and dialysis disequilibrium are dialysis-related complications.
Investigations
• Important urinary abnormalities include a fixed specific gravity around 1.010 (isosthenuria) and the presence of broad casts.
• White cells in the urine usually indicate infection but may also occur in renal tuberculosis and papillary necrosis.
• Eosinophils in the urine indicate allergic tubule-interstitial disease while red cell casts suggest glomerulonephritis.
• The common haematological abnormality is a normochromic normocytic anaemia.
• The most consistent biochemical abnormalities are elevated levels of blood urea and creatinine. The level of serum creatinine correlates with the degree of renal impairment. Other biochemical abnormalities include hypocalcaemia, hyperphosphataemia, hyperuricaemia and hyperkalaemia. Bicarbonate levels are reduced.
• Creatinine clearance is important to assess the severity of renal failure.
• A plain radiograph of the abdomen may be useful in determining the kidney size and in the evaluation of obstructive uropathy.
• Renal ultrasound typically shows shrunken kidneys.
• CT is useful in some patients with suspected obstructive nephropathy.
• Transcutaneous renal biopsy is of value particularly in cases associated with normal-sized kidneys. It is particularly useful if renal functions are deteriorating rapidly.
Management
• The management of CRF falls into three parts-
• Investigations to determine the nature of underlying disease and to detect any reversible factors.
• Measures to prevent further renal damage.
• Supportive measures in the form of dialysis or transplantation when required.
• The following measures can be undertaken which will reduce the symptoms and may slow the progression to terminal renal failure.
• Control of hypertension- The blood pressure should be reduced to less than 140/90 mmHg.
• Protein restriction to 40 g/day (with higher amount of essential amino acids).
• Avoidance of high potassium foods.
• Salt restriction is required in most cases.
• Hypocalcaemia and hyperphosphataemia should be treated aggressively. Hypocalcaemia requires treatment with calcitriol and calcium supplementation. Vitamin D supplementation reduces cardiovascular mortality in ESRD patients. Serum calcium should be monitored frequently to avoid hypercalcaemia. Oral calcium carbonate also reduces the bioavailability of dietary phosphates.
• Metabolic acidosis should be corrected with calcium carbonate, and if required, with small doses of sodium bicarbonate.
• Hyperkalaemia usually responds to dietary restrictions.
• Anaemia should be corrected by appropriate addition of iron, folate and vitamin B 12, if required. The treatment of choice for renal failure-associated anaemia is the use of erythropoietin along with iron. Blood pressure should be carefully monitored during erythropoietin therapy. Oral or intravenous iron is needed to maintain adequate iron stores. Target haemoglobin is 11-12 g/dL. Haemoglobin> 13 g/dL has been shown to be associated with increased incidence of cardiovascular mortality.
• If conservative measures are inadequate, haemodialysis may be needed.
• Kidney transplantation offers the possibility of restoring normal kidney functions.
TREATMENT AT DR. SOHAN LAL CLINIC
The integrated POLYCLINIC facility offers patients to select their treatment either from the Department of Homeopathy or from the Department of Medicine.
We provide scientific, research-based, and professional services to people across the world, aiming to achieve the highest success rate.