Aetiology of cirrhosis
• Alcoholic cirrhosis
• Post-necrotic cirrhosis or post-viral cirrhosis
• Hepatitis B • Hepatitis C • Delta hepatitis (hepatitis D) + hepatitis B Chronic autoimmune hepatitis
• Drug-induced cirrhosis
• Methotrexate • Methyldopa, isoniazid • Sulphonamides
• Biliary cirrhosis
• Primary • Secondary
• Non-alcoholic fatty liver disease (NAFLD) • Cardiac cirrhosis • Haemochromatosis
• Wilson's disease • alpha 1 -antitrypsin deficiency • Glycogen storage diseases
• Galactosaemia • Intestinal bypass surgery • Hepatic outflow tract obstruction
• Veno-occlusive disease • Cryptogenic (Idiopathic) cirrhosis
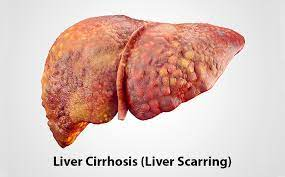
Pathology and Pathogenesis
• Cirrhotic changes affect the whole liver, but not necessarily every lobule.
• Widespread necrosis of liver cells.
• Extensive fibrosis that distorts the hepatic architecture.
• Regenerative, nodular hyperplasia of the remaining surviving liver cells leads to regenerating nodules.
• Destruction and distortion of hepatic vasculature by fibrosis lead to obstruction of blood flow, which eventually leads to portal hypertension and its sequelae.
• Ascites and hepatic encephalopathy result from both hepatocellular insufficiency and portal hypertension.
• Hepatocellular damage leads to jaundice, oedema, coagulopathy and a variety of metabolic abnormalities.
• Alcoholic cirrhosis:
• Safe limits of alcohol are 200 g and 140 g of alcohol per week in males and females, respectively.
• 10 g of alcohol equals 30 mL of whisky, 100 mL of wine and 250 mL of beer.
• Occurrence of cirrhosis six times when alcohol intake is double the safety limit.
• Ingestion of 180 g of alcohol/day for 25 years increases the risk of developing cirrhosis 25 times.
• Hepatitis C infection is an important contributor for progression to cirrhosis.
Clinical Features
Symptoms
• Low-grade fever. • Weakness, fatigue and weight loss. • Anorexia, nausea, vomiting and upper abdominal discomfort. • Abdominal distension due to ascites and gas. • Loss of libido. • Menstrual irregularities like amenorrhoea and irregular menses. • Haemorrhagic tendencies like easy bruising, purpura, epistaxis, menorrhagia and gastrointestinal bleeding. • Haemorrhagic tendencies are due to underproduction of coagulation factors by the liver and thrombocytopenia resulting from hypersplenism. • Symptoms of hepatic insufficiency • Symptoms of portal hypertension and its sequelae
Signs
Signs of hepatocellular failure
• Jaundice • Palmar erythema • Parotid enlargement • Dupuytren's contracture
• Diminished body hair • Clubbing • Spider naevi • White nails • Flapping tremors
• Gynaecomastia • Testicular atrophy • Ascites
Features dominant in alcoholic cirrhosis
• Parotid enlargement • Gynaecomastia • Spider naevi • Dupuytren's contractures (related to alcoholism) • Liver enlarged, normal or small in size
End Stage
• End stage of cirrhosis is characterised by:
• Chronic jaundice.
• Progressive, refractory ascites. Worsening of signs of portal hypertension.
• Progressive renal dysfunction.
• Most of them die in hepatic encephalopathy.
Investigations
• Complete blood picture • Liver function tests
•Prothrombin time • Hepatitis B and C markers • Blood ammonia estimation
• Respiratory alkalosis • Metabolic abnormalities • Ultrasonographic examination
• Fibroscan to determine amount of fibrosis • Liver biopsy confirms the diagnosis of cirrhosis
• Relevant investigations related to the specific aetiologies of cirrhosis in individual patients
• Ascitic fluid examination, barium swallow for demonstration of varices, upper gastrointestinal scopy for delineation of varices
Managment
• Treatment of underlying causes
• Removal of causative agents like drugs, alcohol, etc.
• High-protein diet-minimum 1 g/kg/day.
• 2000--3000 kcal/day.
• Diets enriched in branched-chain amino acids, in patients predisposed to hepatic encephalopathy.
• Multivitamin supplementation daily.
• Vaccination against hepatitis A and B viruses, influenza virus, and pneumococcus.
• Specific treatment of complications-e.g. variceal bleeding, hepatic encephalopathy and ascites
TREATMENT AT DR. SOHAN LAL CLINIC
The integrated POLYCLINIC facility offers patients to select their treatment either from the Department of Homeopathy or from the Department of Medicine.
We provide scientific, research-based, and professional services to people across the world, aiming to achieve the highest success rate.