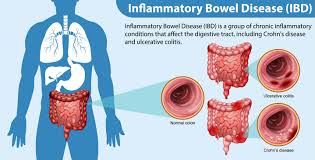
• Inflammatory bowel diseases are chronic inflammatory disorders of gastrointestinal tract characterised by a relapsing and remitting course.
• Inflammatory bowel diseases include several conditions, most common being-
• Ulcerative colitis • Crohn's disease
ULCERATIVE COLITIS
Definition
• Ulcerative colitis is an inflammatory disease affecting mainly the large intestine, characterised clinically by recurrent attacks of bloody diarrhoea and pathologically by diffuse inflammation of colonic mucosa.
Aetiology
• Familial or genetic
• Strong family history
• Occurrence in monozygotic twins
• Infectious
• Possible pathogens include-
*Mycobacterium (M. avium paratuberculosis) *Measles virus
*Listeria monocytogenes *Yeast
* Endogenous bacteria- Bacteroides & E.coli
• Dietary factors
• Deficiency or excess of certain nutrients (butyric acid, sulphides, L-arginine and glutamine)
• Smoking
• Patients with Crohn's disease are more likely to be smokers and smoking can exacerbate it.
• There is an increased risk of ulcerative colitis in non-smokers.
• Psychological
• Characteristic personality and major psychological stresses are related to flare-ups and precipitation of symptoms
Pathology
• Primarily involves the colonic mucosa.
• Mucosa) involvement is uniform and continuous with no intervening areas of normal mucosa.
• Rectum is involved in 95% of cases (proctitis).
• From the rectum the disease extends proximally into the colon in a continuous fashion.
• Back wash ileitis is involvement of a few centimetres of ileum, when the entire colon is involved.
• Macroscopically, the mucosa appears hyperaemic, haemorrhagic or ulcerated. Ulcers do not usually extend deeper beyond the submucosa.
Clinical Features
• Severity of symptoms reflects the extent of colonic involvement and the intensity of inflammation
• Exacerbations and remissions are characteristic
• Bloody diarrhoea with mucus and pus
• Abdominal pain, especially lower abdominal
• Fever, weight loss and loss of appetite
• Symptoms and signs of dehydration and anaemia
Investagations
• Anaemia, raised ESR and leucocytosis • Electrolyte abnormalities
• Hypoproteinaemia • Abnormal liver function tests
• Blood culture in septicaemia • Stool examination and culture to exclude infective pathology
• Barium enema • Sigmoidoscopy
• Colonoscopy • Rectal biopsy shows mucosa! inflammation
Management
• Parenteral nutrition through a central venous line in seriously ill patients
• High-protein and low-residue diet
• Blood and plasma infusions
• Correction of dehydration and electrolyte imbalance
• Correction of septicaemia
CROHN’S DISEASE
Definition
• Crohn 's disease is characterised by patchy and transmural inflammation, which may affect any part of the gastrointestinal tract.
• It may be defined by location (terminal ileal, colonic and ileocolic, upper gastrointestinal) or by pattern of disease (inflammatory, fistulating or stricturing)
Aetiology
• Factors listed under "ulcerative colitis".
Pathology
• Affects small and large bowels, but more common in small bowel. Can affect any part of the gastrointestinal tract from mouth to anus.
• Inflammation extends through all the layers of the intestinal wall.
• Characteristically the involvement is discontinuous. Involved segments of intestine are separated from each other by intervening segments of normal bowel.
• Bowel wall is greatly thickened and leathery with the lumen narrowed (stenosis).
• Mucosa has a nodular cobble stoned look.
Clinical Features
• Chronic disease with exacerbations and remissions
• Young adults with history of fatigue, weight Joss, diarrhoea, fever and pallor
• Abdominal pain occur due to peritoneal involvement or intestinal obstruction
• Right lower quadrant pain, tenderness, guarding and mass
• Mass palpable per abdomen and rectally reflects adherent loops of intestine and abscess
• Recurrent episodes of colicky abdominal pain with nausea, vomiting and excessive borborygmi suggest subacute intestinal obstruction
• Stool usually does not contain frank blood, mucus or pus unless colon is involved
Investigations
• Normochromic normocytic or macrocytic or hypochromic anaemia
• Raised ESR and leucocytosis
• Abnormal liver function tests
• Hypoproteinaemia
• Stool culture and routine examination to exclude infectious causes of diarrhoea
• Schilling test for malabsorption of vitamin B 12
• Sigmoidoscopy and colonoscopy
• Barium meal follow through and barium enema
Management
• Diet and nutrition
• High-protein and high-energy diet
• Enteral feeding by nasogastric tube. Total parenteral nutrition in very ill patients
• Plasma or blood transfusion
• Low residue diet in colic and subacute obstruction
• Low-fat diet and low linoleic acid in diet
• Milk-free diet in lactose intolerance
• Treatment for bacterial colonisation of gut
• Supplementation of iron, folic acid, calcium, zinc, vitamins D, B 12, and electrolytes
TREATMENT AT DR. SOHAN LAL CLINIC
The integrated POLYCLINIC facility offers patients to select their treatment either from the Department of Homeopathy or from the Department of Medicine.
We provide scientific, research-based, and professional services to people across the world, aiming to achieve the highest success rate.