

• In India, common among communities like Sindhi, Punjabi, Gujarat, Parsee. Less common in South India.
Clinical Features
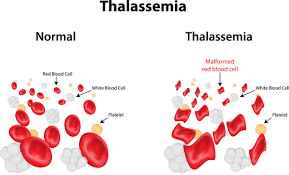
• Severe anaemia (usually develops at 6-24 months of age) and its complications. • Growth and development retardation, feeding problems, diarrhoea and irritability. • Splenomegaly, at times massive. • Hepatomegaly. • Bone marrow hyperplasia resulting in deformities of long bones of legs and craniofacial changes (bossing of the skull, prominent malar eminence, depression of bridge of nose, tendency to a mongoloid slant of the eye and hypertrophy of the maxillae, which tends to expose the upper teeth). • Development of masses from extramedullary haematopoiesis. Paraspinal masses may produce cord compression. • Increased risk of thrombosis particularly in patients who are non-transfused or infrequently transfused and in patients who are splenectomised. • Deposition of iron in tissues (haemosiderosis) resulting in organ failure.
Management
Folic acid supplementation. • Repeated blood transfusions to maintain Hb > 10 gm/dL. Regular transfusions suppress erythropoiesis to provide prevention of skeletal deformities and splenomegaly, and inhibit increased gastrointestinal iron absorption. • Desferrioxarnine therapy to chelate iron and enhance iron excretion. Indicated if serum ferritin > 1500 µ.g/L. Deferiprone and deferasirox are oral iron chelators. • Splenectomy is indicated in children with massive symptomatic splenomegaly, and those with progressively increasing transfusion requirements (above 200-250 mL/kg/year of packed red blood cells). • Allogenic bone marrow transplantation in young patients. • Management of associated complications like congestive heart failure and endocrinopathies.
Leave a Comments