Introduction
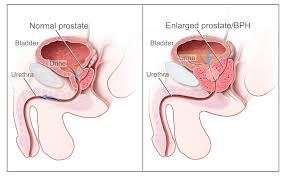
Benign prostatic hyperplasia (BPH), also called prostate enlargement, is a noncancerous increase in size of the prostate gland. The underlying mechanism involves the prostate pressing on the urethra thereby making it difficult to pass urine out of the bladder.
Risk factors include a family history, obesity, type 2 diabetes, not enough exercise, and erectile dysfunction.
BPH typically begins after the age of 40. Half of males age 50 and over are affected. After the age of 80, that figure climbs to as high as about 90% of males affected. Although prostate specific antigen levels may be elevated in males with BPH, the condition does not increase the risk of prostate cancer.
Symptoms & Signs
BPH is the most common cause of lower urinary tract symptoms (LUTS), which are divided into storage, voiding, and symptoms which occur after urination.
Storage symptoms include the need to urinate frequently, waking at night to urinate, urgency (compelling need to void that cannot be deferred), involuntary urination, including involuntary urination at night, or urge incontinence (urine leak following a strong sudden need to urinate). Voiding symptoms include urinary hesitancy (a delay between trying to urinate and the flow actually beginning), intermittency (not continuous), involuntary interruption of voiding, weak urinary stream, straining to void, a sensation of incomplete emptying, and uncontrollable leaking after the end of urination. These symptoms may be accompanied by bladder pain or pain while urinating, called dysuria.
Bladder outlet obstruction (BOO) can be caused by BPH. Symptoms are abdominal pain, a continuous feeling of a full bladder, frequent urination, acute urinary retention (inability to urinate), pain during urination (dysuria), problems starting urination (urinary hesitancy), slow urine flow, starting and stopping (urinary intermittency), and nocturia.
BPH can be a progressive disease, especially if left untreated. Incomplete voiding results in residual urine or urinary stasis, which can lead to an increased risk of urinary tract infection.
Diagnosis
The clinical diagnosis of BPH is based on a history of LUTS (lower urinary tract symptoms), a digital rectal exam, and exclusion of other causes of similar signs and symptoms. The degree of LUTS does not necessarily correspond to the size of the prostate. An enlarged prostate gland on rectal examination that is symmetric and smooth supports a diagnosis of BPH. However, if the prostate gland feels asymmetrical, firm, or nodular, this raises concern for prostate cancer. Uroflowmetry is done to measure the rate of urine flow and total volume of urine voided when the subject is urinating.
Abdominal ultrasound examination of the prostate and kidneys is often performed to rule out hydronephrosis and hydroureter. Incidentally, cysts, tumours, and stones may be found on ultrasound. Post-void residual volume of more than 100 ml may indicate significant obstruction. Prostate size of 30 cc or more indicates enlargement of the prostate.
Management
When treating and managing benign prostatic hyperplasia, the aim is to prevent complications related to the disease and improve or relieve symptoms.
Lifestyle
Lifestyle alterations to address the symptoms of BPH include physical activity, decreasing fluid intake before bedtime, moderating the consumption of alcohol and caffeine-containing products and following a timed voiding schedule.
Physical activity
Physical activity has been recommended as a treatment for urinary tract symptoms.
Voiding position
Voiding position when urinating may influence urodynamic parameters (urinary flow rate, voiding time, and post-void residual volume). A meta-analysis found no differences between the standing and sitting positions for healthy males, but that, for elderly males with lower urinary tract symptoms, voiding in the sitting position-
*decreased the post void residual volume;
*increased the maximum urinary flow, comparable with pharmacological intervention; and
*decreased the voiding time.
This urodynamic profile is associated with a lower risk of urologic complications, such as cystitis and bladder stones.
TREATMENT AT DR. SOHAN LAL CLINIC
The integrated POLYCLINIC facility offers patients to select their treatment either from the Department of Homeopathy or from the Department of Medicine.
We provide scientific, research-based, and professional services to people across the world, aiming to achieve the highest success rate.to achieve the highest success rate.