BRONCHIAL ASTHMA
DEFINATION
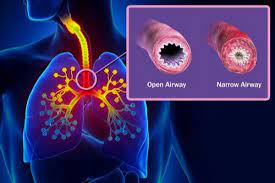
• Bronchial asthma is a heterogeneous disease, usually characterised by chronic inflammatory disease of the airways. It is defined by history of dyspnoea, cough, chest tightness and wheezing, that vary over time and in intensity, together with variable expiratory airflow limitation. It results from narrowing of the airways produced by a combination of muscle spasm, mucosa! oedema and viscid bronchial secretion. The airflow limitation is generally reversible spontaneously or with treatment.
• Asthma is usually associated with bronchial hyper-reactivity so several stimuli.
• Asthma-COPD overlap syndrome is characterised by persistent airflow limitation with several features usually associated with asthma as well as COPD.
CLASSIFICATION
• Bronchial asthma can be classified into two main groups or phenotypes:
1. Early-onset asthma (atopic, allergic and extrinsic).
2. Late-onset asthma (non-atopic, idiosyncratic and intrinsic)
AETIOPATHOGENESIS
• Pathogenesis of asthma involves two major factors:
1. Bronchial hyper-responsiveness.
2. Inflammatory reaction within bronchial wall.
Role of Allergens
• The allergens responsible for asthma enter the body through various routes:
• Inspired air (house dust, pollen, feather, animal dander, fungal spores, etc.).
• Ingestion (allergens in fish, egg, milk, yeast and wheat).
• Previous exposures to these allergens will have stimulated the formation of IgE. Hence, subsequent exposure to these specific allergens will result in an anaphylactic antigen-antibody reaction in the bronchi.
CLINICAL FEATURES
• Clinical features are conveniently discussed under three headings:
1-Episodic Asthma
• Occurs as episodes with asymptomatic intervening periods.
• Characterised by paroxysms of wheeze and dyspnoea with relatively sudden onset.
• Episodes may be spontaneous in onset or triggered by allergens, exercise or viral infections.
• Attacks may be mild or severe and may last for hours, days or even weeks.
2-Severe Acute Asthma (Status Asthmaticus)
• It is a condition in which severe airway obstruction and asthmatic symptoms persist despite the initial administration of standard acute asthma therapy.
• Severe dyspnoea and unproductive cough.
• Patient adopts an upright position fixing the shoulder girdle to assist the accessory muscles of respiration.
• Physical signs include sweating, central cyanosis, tachycardia and pulsus paradoxus.
3-Chronic Asthma
• Symptoms are usually chronic unless controlled by appropriate therapy.
• Symptoms like chest tightness, wheeze and breathlessness occur on exertion.
• Episodes of spontaneous cough and wheeze occur during the night.
• Repeated attacks of "severe acute asthma" are common.
• Chronic cough with mucoid sputum, punctuated by recurrent attacks of purulent expectoration from frank infection, is a common feature of chronic asthma.
Physical Signs in the Chest
• During an attack of asthma, the following signs are detectable:
• Respiratory rate is increased with the use of accessory muscles of respiration.
• Breath sounds are vesicular in character with prolonged respiration.
• Numerous high-pitched polyphonic expiratory and inspiratory rhonchi are audible.
• During very severe attacks the airflow may be insufficient to produce rhonchi. This results in a "silent chest", which is an ominous sign.
• In between the attacks, the chest is clear and no abnormal physical signs may be detectable.
• Chronic asthmatics usually have some scattered rhonchi always persisting in their chest.
INVESTIGATIONS
• Chest radiography:
• In an acute attack, lungs appear hyperinflated.
• In between attacks, lungs look normal.
• Long-standing cases have hyperinflated lungs indistinguishable from emphysema.
• Complications like pigeon chest, lobar or segmental collapse, pneumothorax and mediastinal and subcutaneous emphysema may be seen.
• Pulmonary function tests.
• ABG analysis shows hypoxaemia and hypocarbia during acute attack. In severe acute asthma, hypercarbia develops.
• Skin hypersensitivity tests.
• Sputum and blood eosinophilia.
• Elevated serum IgE levels.
MANAGEMENT OF BRONCHIAL ASTHMA
• Goals of asthma management are:
• To achieve good control of asthma symptoms and maintain normal activities.
• To minimise future risk of exacerbation, fixed airflow limitation and medication side effects.
• Management of bronchial asthma can be discussed under following broad headings-
1. Avoidance of allergens. 2. Modify risk factors for exacerbation.
3. Desensitisation or immunotherapy. 4. Drug therapy to control or suppress clinical manifestations.
Modify Risk Factors for Exacerbation
• Cessation of smoking; avoidance of passive smoke inhalation. • Control of associated rhinitis.• Control obesity. • Inadequate use of inhaled corticosteroids. •Avoid overuse of inhaled short-acting beta-agonists. •Poor inhalation technique. •Avoid major psychological problems.
TREATMENT AT DR. SOHAN LAL CLINIC
The integrated POLYCLINIC facility offers patients to select their treatment either from the Department of Homeopathy or from the Department of Medicine.
We provide scientific, research-based, and professional services to people across the world, aiming to achieve the highest success rate.