The condition is defined as a long standing chronic suppuration of the middle ear cleft and its muco-periosteal lining resulting in discharging ear and deafness.
The disease has its origin in following ways:
1. Few attacks of acute middle ear infection which has failed to resolve completely.
2. Some cases are traceable to acute infectious diseases of childhood such as measles, influenza, diphtheria, etc.
3. Insiduous chronic keratinising process seen in attic and postero-superior part of the tympanic membrane.
4. Disorder of ventilation and Retraction-pocket formation.
5. Long standing secretory otitis media.
6. Bacteriological: pseudomonas, staphylococcus, proteus, E. coli infection change the pathology of the middle ear cleft.
Factors responsible for chronicity are following:
1. Poor drainage of inflammatory exudate.
2. Eustachian tube dysfunction.
3. Aerobic and anaerobic flora.
4. Antibiotic resistant strain and also failure of antibiotic to penetrate exudate.
5. Osteitis and granulation tissue blocking drainage.
6. Presence of keratinising squamous epithelium and debris helps growth of organism and also cholesteatoma formation.
7. Diffuse mucosal changes with scarring and devascularisation.
8. Immuno-deficiency.
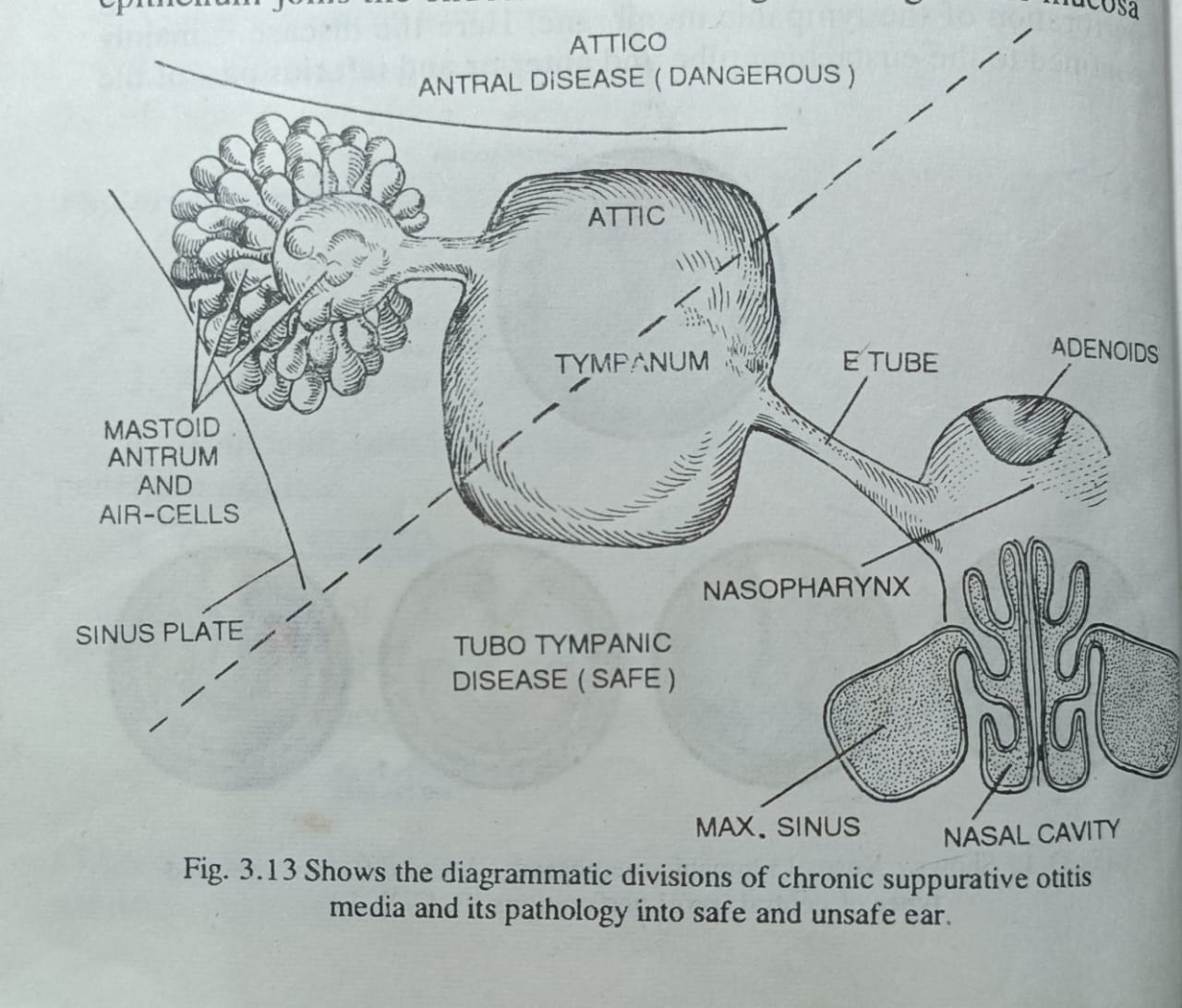
Clinico-pathologically the disease is divided into two different varieties
2. Tympano-mastoid type or Attico antral variety. This is normally unsafe or dangerous variety and runs aggressive course. If untreated, it causes destruction of middle ear and mastoid bone and produces various complications.
TUBO TYMPANIC DISEASE OR SAFE VARIETY OF C.S.O.M
Aetio-Pathology: This usually starts in childhood and is usually a complication of acute otitis media where there is persisting perforation of the tympanic membrane. Here the disease is mainly confined to the eustachian tube and anterior and inferior part of the tympanic cavity. The drum perforation is central ie margin is formed by pars tensa all around. It may be in the anterior or posterior segment and of various size or shape. In advanced case it may be subtotal perforation of the pars tensa with often erosion of handle of the malleus. Recurrent infection of the middle ear occurs through the eustachian tube from the naso-pharynx, nose, and sinuses or via the external auditory canal through the perforation. The perforation does not heal as the squamous epithelium joins the endothelium all along the margin. The mucosa of the middle ear is pink and velvety, but may be oedematous and polypoid in some cases. The epithelial lining in tubo-tympanic region is mainly ciliated columnar epithelium which contains secretory cells (goblet cells and mucous glands) and that is why the discharge in this type of disease is profuse and mucoid. The drainage is also good. As the chance of cholesteatoma formation is insignificant, there is no bone erosion and the discharge is not foul smelling. Chances of complications are unlikely.
Predisposing factors:
1. Recurrent upper respiratory tract infection, nasal allergy, chronic rhino-sinusitis, etc.
2. Enlarged adenoids in children, chronic tonsillitis, etc.
3. Bathing and swimming in pools, picking of the car with infected material, etc.
4. Malnutrition and hypogummaglobinaemia.
Clinical features:
1. Recurrent otorrhoea discharge is watery or mucoid and sometimes mucopurulent in character; may be profuse, but non foetid. The ear is dry in between infection.
2. Deafness: deafness is progressive unless disease is controlled early. This is conductive type, usually mild to moderate in degree, depending on the site and size of perforation.
3. Pain: is usually absent, but may be present due to secondary infection or associated otitis externa.
4. Otoscopy shows perforation of the tympanic membrane- central in type and varies in shape and size. Sometimes the eustachian tube opening can be seen through big anterior or subtotal perforation. Middle ear mucosa is often found to be pink and velvety. Occasionally oedematous mucosa may protrude through a perforation as a polyp which is pale.
5. Source of infection is often seen in the nose or pharynx (rhinitis, sinusitis, enlarged adenoids or tonsillitis), which is the cause of persistence of disease.
Tuning fork test: Rinne is negative and Weber is lateralised to the diseased side (conductive deafness). In cases of bilateral lesions, Weber is lateralised to the more deaf ear.
Audiogram: confirms conductive deafness with A-B gap.
Radiology: Mastoid is usually cellular, but may be hypocellular. There is no evidence of bone erosion.
Course of the disease: can be divided into stages.
(a) Active stage: when the ear is actively discharging.
(b) Quiescent stage: when the ear is not discharging for sometime, but history of otorrhoea in the recent past.
(c) Inactive stage: H/o past otorrhora, but when the ear is dry for a significant period upto 3-6 months.
(d) Healed stage: when the perforation has healed up with or without adhesive change and ear is permanently dry.
Management- aim is to keep the ear dry.
1-Precautions and instructions to patients:
(a) Avoid entry of water in ear. Ear is plugged with cotton wool impregnated with vaselene or ear obturator, when hair is washed.
(b) Avoid swimming and diving.
(c) Maintain aural hygiene and avoid cleaning of ear discharge with dirty cotton or linen.
(d) Tetanus immunisation is essential among villagers and slum dwellers to prevent otogenous infection.
2- General nutrition: is to be improved with good food and vitamins in cases of undernourished children.
TREATMENT AT DR. SOHAN LAL CLINIC
The integrated POLYCLINIC facility offers patients to select their treatment either from the Department of Homeopathy or from the Department of Medicine.
We provide scientific, research-based, and professional services to people across the world, aiming to achieve the highest success rate.